Diagnosis
General Practitioners may diagnose Addison’s disease through reviewing the patient’s medical history and current symptoms, they may also ask about the patient’s family relatives- to see if there are any family histories of autoimmune disorders.
Assessments for clinical signs includes:
- Measurement of blood pressure whilst sitting and standing using a sphygomomanometer (blood pressure measurement). Postural hypotension usually results in a 20mmHg drop in blood pressure whilst standing. Orthostatic hypotension (low blood pressure when changing positions) is also measured.
- Patients are questioned about their daily activities (such as carrying heavy shopping bags) to establish if they are suffering from proximal myopathy or overall muscle weakness.
- Inspection for patchy hyperpigmentation or pigmentation of the palmar creases (although not present in all cases) and scars is performed. Hyperpigmentation generally occurs in areas of increased friction and may be visible where clothes rub against the skin or on the oral mucosa, depending on the patient’s natural level of melanocytes.

Blood pressure measurement using a sphygomomanometer modified image courtesy of Flickr under the creative commons license.
Measurements for blood cortisol
However a one-off measurement of blood cortisol is not good enough to diagnose Addisons disease, as cortisol levels may be low from time to time in normal people. Therefore if Addison’s disease is suspected a special stimulation test is needed to confirm the diagnosis. The adrenal gland can be ‘stimulated’ by an injection of a drug similar to ACTH. If the adrenals are normal, then blood samples taken after the injection should show a rise in cortisol. If you have Addison’s disease you do not have a rise in blood cortisol following the injection. Also a blood test can sometimes detect antibodies, which cause autoimmune Addison’s disease.
The cortisol test is measured using urine samples or a blood sample from the patient’s vein is also performed.
As well as looking for low cortisol levels, blood samples are also used to detect the following:
- A low level of sodium, potassium, glucose or aldosterone.
- A high level of ACTH.
These observations can also be used to test for Addison’s disease; however a Synacthen stimulation test is later performed to confirm the diagnosis.
Synacthen stimulation test
Is a safe test, usually conducted by a general practitioner or secondary care via referral. Synacthen is a synthetic copy of ACTH (which is usually naturally produced by the pituitary gland, to encourage the adrenal gland to release the hormone cortisol and aldosterone). By administrating synacthen the adrenal gland should respond in the same way as if it were real ACTH, and release cortisol and aldosterone into the blood.
A blood sample is taken to test the level of cortisol and aldosterone. Synacthen is usually administrated through injection into the arm. After 30 minutes another blood sample is taken followed by further blood samples every half an hour for up to two hours. Patients with either form of adrenal insufficiency respond poorly or do not respond at all.

Needle used for hormone replacement courtesy of Flickr under the creative commons license.
CHR Stimulation Test
When response to the short ACTH test is abnormal a ‘long’ CRH stimulation test is required to determine the cause of adrenal insufficiency. In this test synthetic CRH is injected intravenously and blood cortisol is measured before and after 30, 60, 90 and 120 minutes after injection. Patients with primary adrenal insufficiency have high ATCHs but are unable to produce cortisol. Patients with secondary and adrenal insufficiency have deficient cortisol responses but absent or delayed ACTH responses. These observations can be explained through absent ACTH response points to the pituitary.
Plasma renin activity is raised in Addison’s disease and its measurement is also sometimes useful in differentiating between Addison’s disease and secondary adrenal insufficiency.
The blood samples are often tested for cortisol, aldosterone and ACTH. If ACTH level is high but cortisol and aldosterone levels are low, it is suggested that the patient is suffering from Addison’s disease.
Medical imaging
Medical imaging includes ultrasounds, computed tomography or magnetic resonance imaging.
X-ray exams of the adrenal and pituitary glands may also be useful to help understand the underlying cause to Addison's disease. However these x-rays or ultrasonic scan of the adrenals is most likely to only show calcification, and is therefore probably not useful unless there is a strong suspicion of TB. Adrenal antibodies are likely to be positively associated with Addison’s disease but this cannot always be seen.
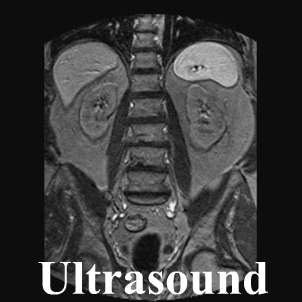
Ultrasound image of the adrenal glands modified image courtesy of Flickr under the creative commons license.
Diagnosis for patients suffering from adrenal crisis
During an adrenal crisis, your blood pressure will be dangerously low, and your symptoms will be very severe. In these situations, there is not enough time to perform a synacthen stimulation test to confirm whether you are suffering from Addison’s disease, therefore it is important that the doctor must begin treatment with injections of salt, fluids and glucocorticoid hormones immediately.
Although a reliable diagnosis is not possible while the patient is being treated for the crisis, measurements of blood ACTH and cortisol during the crisis is used to make a diagnosis. Once the crisis is controlled and medication has been stopped, the doctor will continue further testing for up to 1 month to obtain accurate results of the condition.